Big news is shaking up the medical world! The U.S. Food and Drug Administration (FDA) has just approved a groundbreaking, long-lasting injection to prevent HIV. This development is more than just a scientific win—it’s a beacon of hope for millions at risk of HIV infection. Let’s dive into what this exciting approval means, how it works, and why it just might change everything we know about HIV prevention.
The Long-Awaited News: What Did the FDA Approve?
Great advancements in HIV prevention have been made over the past few decades, but daily medications and strict regimens remain the norm for those at risk. That all changed when the FDA gave the green light to the first-ever long-acting injectable for HIV pre-exposure prophylaxis (PrEP). This new injectable is ushering in a new era where preventing HIV doesn’t have to be a daily hassle.
The medication, called cabotegravir and branded as Apretude, is injected once every two months—no more pill-a-day anxiety, no more missed doses due to a busy schedule. By simplifying prevention, this approval could make a remarkable difference in the fight against the spread of HIV.
How Does the HIV Prevention Injection Work?
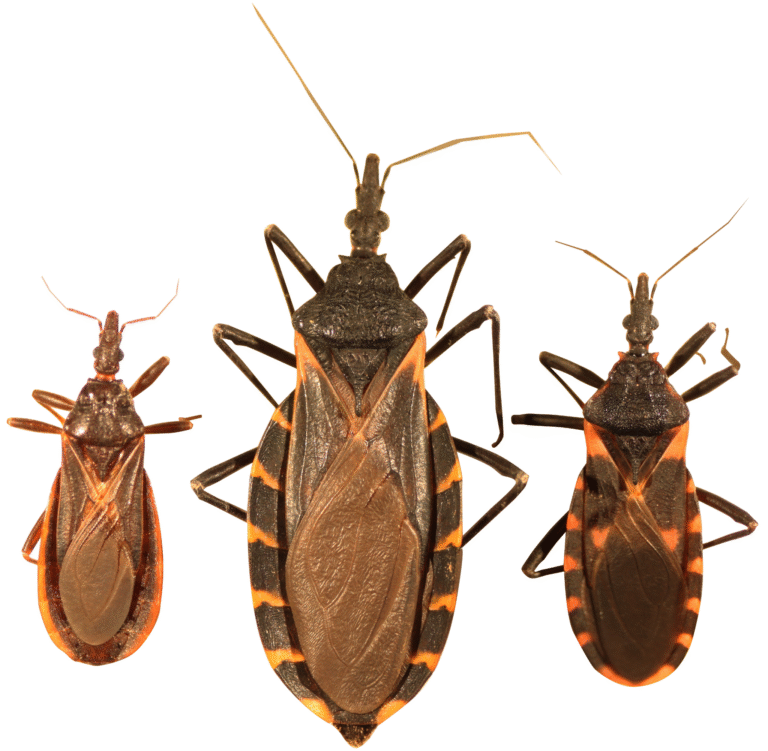
The mechanics behind cabotegravir are both elegant and powerful. As a long-acting integrase strand transfer inhibitor (INSTI), cabotegravir works by blocking a key enzyme that the HIV virus needs to replicate inside the body. By stopping this enzyme, the drug provides a barrier that prevents the virus from establishing an infection, even if someone is exposed.
What sets this injection apart is its extended protective power. By keeping therapeutic drug levels consistent for two months at a stretch, cabotegravir wipes out the worry of remembering daily pills. This could be particularly meaningful for individuals whose lives are hectic or unpredictable.
Why a Long-Lasting PrEP Option Changes the Game
Anyone who’s ever tried keeping up with daily medication knows it’s trickier than it sounds. Life gets busy; routines get interrupted. For people at risk of HIV, missing even just a few doses of preventative medicine can open the door to infection.
By moving to a once-every-two-months injection, the barriers to effective HIV prevention drop dramatically. There’s less stigma than remembering to take a pill, more privacy, and greater freedom for those who want safe, reliable protection. Plus, healthcare providers can track and ensure patients get their protective doses on schedule.
Who Stands to Benefit?
Although this breakthrough is great news for everyone, it offers special promise for:
Individuals at high risk for HIV include men who have sex with men, transgender women, and heterosexual individuals in high-risk relationships.
People who have trouble adhering to daily oral PrEP.
Communities with limited access to healthcare or where daily medication is less feasible due to life circumstances or stigma.
This injection won’t be for everyone, but it offers an alternative that could close gaps in protection and eliminate major hurdles for many.
What Does the Approval Process Mean?
FDA approval is no small feat! For a drug to reach this milestone, it must prove itself in rigorous, large-scale clinical trials. In the case of cabotegravir, studies showed it was highly effective in reducing the risk of HIV transmission, more so than daily pills! Safety profiles were positive, side effects manageable, and participants overwhelmingly preferred the convenience of the injection.
Rolling Out the Injection: What to Expect
Now that the FDA has approved it, health clinics across the country are gearing up to offer this innovative prevention method. Medical teams will educate patients about the benefits and possible side effects, administer injections, and provide the supportive care needed for successful PrEP.
While the injection won’t eliminate the need for comprehensive safe-sex practices and regular health screenings, it expands the toolkit for HIV prevention.
The Broader Impact: Public Health and Prevention
Injectables like cabotegravir could be transformative not only for individuals but also for public health as a whole. By making HIV prevention easier, more accessible, and more discreet, we could see a real decline in new infections. For at-risk communities, marginalised groups, and those facing healthcare barriers, this approval marks a step toward closing persistent health disparities.
Moreover, people who previously avoided daily pills—whether out of fear, inconvenience, or stigma—might now feel empowered to take control of their health in a whole new way.
Looking Ahead: Challenges and Opportunities
Of course, no innovation comes without a few hurdles. Healthcare providers and policymakers must work together to ensure:
The injection is covered by insurance or assistance programs, so it’s accessible to everyone who needs it.
Clinics and healthcare centres are equipped and trained to deliver the injections safely and efficiently.
Communities are educated and empowered to understand their options and make informed decisions.
However, with the FDA’s stamp of approval and the support of the medical community, these challenges are ones we can take on with optimism!
Frequently Asked Questions (FAQ)
Q: How effective is the injection compared to daily PrEP pills?
A: Clinical trials showed the injectable was at least as effective—and possibly more so—than daily oral PrEP at preventing HIV infection when used as directed.
Q: How often do you need to get the shot?
A: After two initial injections a month apart, you’ll receive the shot once every two months. That’s just six injections a year for ongoing protection.
Q: Are there any major side effects?
A: Most people tolerate the injection well. Some may experience mild soreness at the injection site, headaches, or fatigue. Severe side effects are very rare. Your healthcare provider can discuss any risks with you.
Q: Is this method suitable for everyone?
A: The injection is approved for adults and adolescents weighing at least 77 pounds who are at risk of HIV infection. However, your doctor will help you decide if it’s the right prevention strategy for you.
Q: Will it be affordable?
A: The hope is that insurance plans, Medicaid, and patient assistance programs will make the injection widely accessible. Talk to your provider or local public health clinic about options.
Q: Does it replace safe sex and regular testing?
A: No! The injection is a powerful tool, but it’s best used alongside other preventative measures like condoms and regular HIV screening.
My Reflections as a Health Communicator
Watching this approval unfold gives me goosebumps. I remember a time when HIV prevention was complicated, and hope seemed in short supply. Now, there’s an option that fits modern life, with the potential to save lives, stop the spread, and inspire even greater advances. There’s still work to be done—making this medicine available, affordable, and accessible to all. But right now, let’s appreciate this joyful step forward, knowing that science, steadfast dedication, and community voices really can change the world.
Final Thoughts
What does the future hold? Maybe a world where HIV is no longer a threat at all. Until then, milestones like this FDA approval keep us moving forward. If you or someone you know could benefit from this new prevention option, reach out to a healthcare provider. Let’s spread the good news—and keep working together for a healthier, safer future.