Symptoms of Psychosis
Hallucinations
Hallucinations are false sensory experiences that happen without oncoming stimuli. They can be experienced through any of the five senses, but most typically manifest themselves through auditory (hearing voices) or visual (seeing people or objects) experiences.
Auditory Hallucinations: “Hearing voices” that may comment on a person’s actions, argue or give orders. Voices can also be threatening or neutral.
Visual Hallucinations: The perception of light, shadows, or even whole figures that are not visible to others.
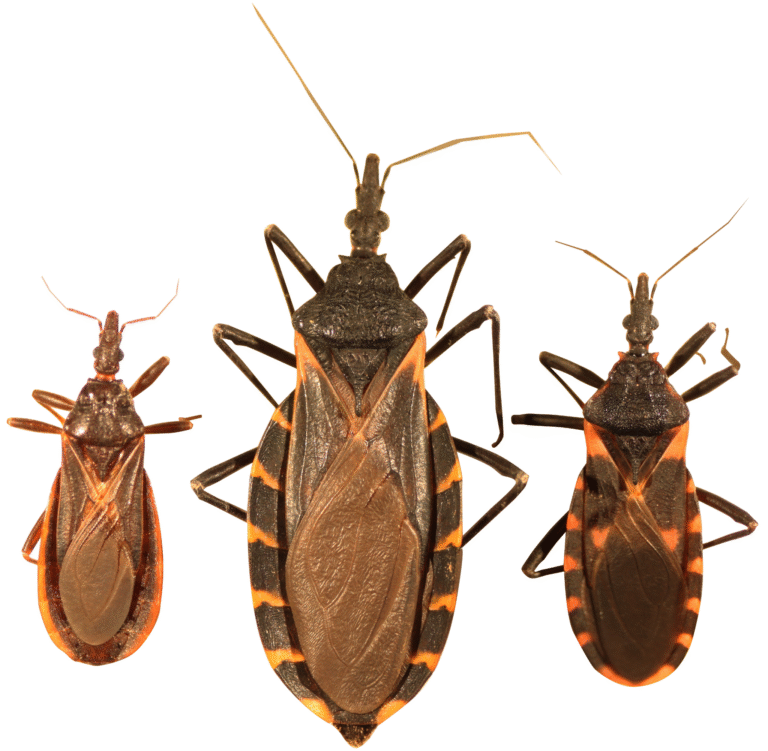
Tactile/Olfactory Hallucinations: єE.g., feeling bugs crawling on the skin or smelling something that has no source.
If so, can these hallucinations feel so real that researchers are unable to tell the difference from reality?
Delusions
These are fixed, false beliefs that cannot be reasoned with. Common types include:
Persecutory Delusions: Where one believes they are being monitored, tracked, or harmed (e.g., “The government is spying on me”).
– Grandiose Delusions: Exaggerated self-importance (e.g., “I am a god with unique powers”).
Referential Delusions: Giving personal meaning to neutral events (e.g., “The TV anchor is sending me secret messages”)
Somatic Delusions: A false belief concerning the function or appearance of one’s body (e.g., “My organs are rotting”)
Disorganized Speech and Thinking
Certain speech patterns are used in thought disorders, for example:
Tangentiality: Wandering off-topic mid-sentence.
Word Salad. Random garbage words.
Circumstantiality: Specifically references that get around to a point.
This symptom is indicative of underlying confusion and compromised logical processing.
Disorganized or Catatonic Behavior
Behaviors can get random or meaningless, for instance:
Of agitation, aggression, or erratic movements
—Catatonia (staying immobile for hours).
Exposing oneself in public (e.g., taking off people’s clothes in public).
These behaviours are not unusual, as they derive often from acute internal overstimulation or broken thought.
Causes and Risk Factors
Psychosis is at least partly due to a combination of biological, psychological and environmental factors:
Mental Health Disorders
− Schizophrenia − More than six months of psychosis, usually with negative signs (i.e. also the absence of motion)
Bipolar Disorder: Manic or depressive episodes can have psychotic features.
Major Depressive Disorder with Psychotic Features: The experience of severe depression combined with delusions or hallucinations.
Substance-Induced Psychosis
Drugs like meth, LSD or cannabis can cause it to occur temporarily. Alcohol withdrawal, or heavy use over a long period, may also play a role.
Medical Conditions
People with infection: HIV/AIDS, encephalitis, or untreated syphilis.
Metabolic Imbalances: Extreme electrolyte abnormalities or Thyroid dysfunction
Trauma and Stress
Psychosis may be provoked in susceptible individuals by childhood trauma (which some research suggests is particularly effective if the trauma is sexual), PTSD or acute stress (for instance, grief).
Genetic Factors
A strong family history of psychosis is a risk factor. Certain genes (ex: COMT, DISC1) correlate with neurotransmitter dysregulation.
Diagnosis and Treatment
Diagnosis involves:
Clinical Interviews: Inquiry on symptoms, medical history, and substance use.
Physical Exams and Tests — May include bloodwork, MRI or EEG to rule out medical causes
Mental Assessment: Identifying underlying disorders using the DSM-5.
Treatment Options:
Antipsychotic Medications
First-Gen (Typical): Haloperidol, Chlorpromazine (Antagonize dopamine receptors).
Second-Generation (Atypical): Risperidone, Quetiapine (act on serotonin and dopamine).
Common side effects include weight gain, drowsiness or movement disorders.
Psychotherapy
Cognitive Behavioral Therapy (CBT): Assists in disputing delusional beliefs.
Family Therapy: Teaches families how to support their loved ones.
Social and Community Support
Early Intervention Programs: To help young adults postpone or avoid full-boil psychosis.
Supported Employment/Education: Assist with re-entering normal life
Hospitalization
It is important in times of intense episodes to maintain safety.
FAQs About Psychosis
- Are psychosis and schizophrenia the same?
No. Psychosis is a symptom, while schizophrenia is a chronic disorder that involves psychosis and other symptoms (e.g., cognitive deficits).
- Can psychosis be cured?
Some recover completely, especially with swift treatment. Some cope long-term with symptoms. Psychosis induced by substances can often resolve with detox.
What to Do When Someone Is Having a Psychotic Episode
This should not be a confrontational situation, so get out if you can, stay calm if you cannot and do your best to stay safe. [0:22] Addressing mental health concerns — Encourage them to seek help from a professional and reassure them that their mental health is valid.
Is there a connection between psychosis and psychopathy?
No — psychopathy is about traits that reach antisocialism; psychosis is about distortions of reality.
- Can children develop psychosis?
Yes, though rare. It could indicate developmental disorders or trauma.
This Site Uses Cookies By continuing, you agree to their use.
Can be from days (brief psychotic disorder) to months. Time will shorten if you treat early.
- Do medications always work?
Many respond well, but a lot is trial and error. For treatment-resistant cases, clozapine is used.
Conclusion
Psychosis is a complex condition that needs to be treated holistically. We now know that thanks to therapies in psycho-pharmacology and psychiatry, a great many people recover or lead meaningful lives with good symptom management. We also need to raise awareness and reduce stigma — to create supportive environments for those affected. If you or someone you know is showing signs of psychosis, please seek medical attention immediately—treatment can make a world of difference. Read more